Hip ORIF Physical Therapy Protocol: An Overview
This protocol provides a guideline for post-operative rehabilitation following hip ORIF․ It aids clinicians in managing patient recovery, integrating exercises, pain management, and functional activities to reclaim an active lifestyle․
Hip ORIF, or Open Reduction and Internal Fixation, is a surgical procedure commonly employed to address hip fractures, one of the most frequent fracture types seen in emergency departments․ Following a hip fracture, surgical intervention, often involving metal pins, plates, screws, or even hip replacement, aims to stabilize the bone; Post-surgery, rehabilitation is crucial for regaining function and independence;
This rehabilitation process, guided by physical therapy, focuses on a structured progression of exercises and activities․ The goal is to restore range of motion, strength, balance, and gait․ This comprehensive approach, tailored to individual needs and recovery timelines, helps patients transition from hospital care to home exercise programs․ Effective physical therapy minimizes complications and maximizes the potential for a return to pre-injury activity levels․
Initial Post-Operative Phase
The initial phase prioritizes early mobilization, pain management, wound care, and infection prevention․ Exercises begin within 24 hours, focusing on gait training, quad sets, and straight leg raises, as instructed․
Early Mobilization and Weight-Bearing Guidelines
Early mobilization following a hip ORIF is crucial for preventing complications and promoting healing․ Weight-bearing guidelines are typically determined by the surgeon based on fracture stability and fixation method․ Initially, patients may be non-weight-bearing (NWB) or toe-touch weight-bearing (TTWB) on the operated leg, utilizing assistive devices like walkers or crutches․
Physical therapy begins within the first 24-48 hours, focusing on bed mobility exercises such as ankle pumps and gentle isometric contractions․ Transitioning from bed to standing is practiced, followed by short intervals of standing with support․ As healing progresses, weight-bearing is gradually increased according to the surgeon’s orders, moving from partial weight-bearing (PWB) to full weight-bearing (FWB)․
Gait training is essential, emphasizing proper technique and minimizing compensatory strategies․ Regular monitoring and adjustments are necessary to ensure patient safety and optimal recovery․ Adherence to weight-bearing guidelines is paramount to avoid compromising fracture healing․
Pain Management Strategies
Effective pain management is paramount following a hip ORIF to facilitate participation in rehabilitation and improve overall outcomes․ A multimodal approach is typically employed, combining pharmacological and non-pharmacological interventions․ Pain medication, prescribed by the physician, should be administered as directed, often timed to provide relief prior to therapy sessions․ Patients should communicate the effectiveness of the medication to optimize dosing․
Non-pharmacological strategies include ice or heat application, positioning for comfort, and gentle range of motion exercises to prevent stiffness․ Transcutaneous electrical nerve stimulation (TENS) may also be utilized to modulate pain signals․ Relaxation techniques, such as deep breathing and guided imagery, can help reduce anxiety and improve pain tolerance․
Open communication between the patient, physical therapist, and physician is vital to ensure adequate pain control throughout the rehabilitation process․ The patient’s pain levels must be considered to personalize the exercise program and prevent overexertion․
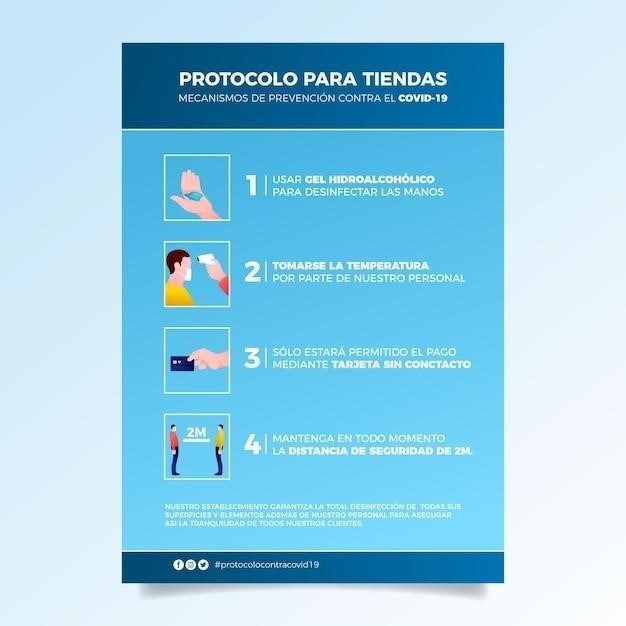
Wound Care and Infection Prevention
Proper wound care is crucial following hip ORIF to prevent infection and promote optimal healing․ The surgical site must be kept clean and dry․ Patients should follow the specific instructions provided by their surgical team regarding dressing changes and wound cleaning procedures․ Regular inspection of the wound for signs of infection, such as increased redness, swelling, warmth, drainage, or pain, is essential․
Patients should be educated on proper hand hygiene techniques to minimize the risk of introducing bacteria to the wound․ Showering is generally preferred over bathing to avoid prolonged soaking of the incision․ Loose-fitting clothing should be worn to prevent irritation and allow the wound to breathe․
Adherence to prescribed antibiotics is critical to prevent infection․ Any fever or signs of infection should be immediately reported to the physician․ Maintaining good nutrition and hydration supports the body’s natural healing processes and strengthens the immune system․ Following these guidelines helps ensure a successful recovery․
Intermediate Rehabilitation Phase
This phase focuses on improving range of motion, strengthening hip and leg muscles, and progressing gait training․ Assistive devices may still be used as needed during this time․
Range of Motion Exercises
Following a hip ORIF, regaining hip range of motion is crucial for functional recovery․ Physical therapy will incorporate exercises to gently restore movement, aiming to improve flexibility and reduce stiffness․ These exercises are typically initiated in the intermediate rehabilitation phase, building upon the early mobilization efforts․
Common range of motion exercises include hip flexion, extension, abduction, adduction, and rotation․ These may be performed passively, with the therapist guiding the movement, or actively-assisted, where the patient contributes to the motion with some therapist support․ Active exercises, where the patient moves the joint independently, are introduced as tolerated․
The progression of range of motion exercises is carefully monitored to avoid overstressing the healing tissues․ Pain levels are closely assessed, and exercises are modified accordingly․ Regular performance of these exercises, as prescribed by the physical therapist, is essential for achieving optimal hip function and preventing long-term limitations․
Remember to follow your therapist’s instructions and avoid pushing through any sharp or severe pain․
Strengthening Exercises for Hip and Leg Muscles
Strengthening the hip and leg muscles is paramount during the intermediate rehabilitation phase after a hip ORIF․ These exercises aim to restore muscle strength, improve stability, and enhance functional abilities․ Strengthening exercises are gradually introduced as pain and healing allow, ensuring proper form and technique to prevent complications․
Common exercises include isometric contractions (muscle activation without movement), such as quad sets and gluteal squeezes․ As strength improves, isotonic exercises (muscle contraction with movement) are incorporated, like hip abduction, adduction, flexion, and extension using resistance bands or light weights․ Leg presses and heel raises may also be included․
The focus is on strengthening the muscles surrounding the hip joint, including the gluteals, quadriceps, hamstrings, and hip flexors․ Strengthening these muscles helps to stabilize the hip, improve gait mechanics, and facilitate a return to daily activities․ Remember that your personal home exercise program should be followed 2-3 times per day․
Gait Training and Assistive Devices
Gait training is a crucial component of the intermediate rehabilitation phase following a hip ORIF․ The goal is to restore a safe and efficient walking pattern while minimizing stress on the healing hip․ Assistive devices, such as walkers or crutches, are often used initially to provide support and reduce weight-bearing forces․
Gait training progresses gradually, starting with partial weight-bearing and advancing to full weight-bearing as tolerated․ Physical therapists guide patients on proper techniques, focusing on step length, cadence, and balance․ Exercises may include weight shifting, forward stepping, and backward stepping․
The use of assistive devices is gradually weaned as strength and balance improve․ The transition from a walker to crutches and then to independent walking is carefully monitored․ Proper footwear and a safe environment are essential․ Gait training aims to optimize mobility and independence, allowing patients to return to their daily activities with confidence․
Advanced Rehabilitation Phase
This phase focuses on restoring full function through activity-specific exercises․ Proprioception and balance exercises are integrated to enhance stability․ The ultimate goal is a safe return to pre-injury activity levels․
Functional Exercises and Activity-Specific Training
In the advanced rehabilitation phase following a Hip ORIF, the emphasis shifts toward functional exercises and activity-specific training․ This stage aims to bridge the gap between basic rehabilitation exercises and the demands of daily life, recreational activities, or sports․ Functional exercises are designed to mimic real-world movements and tasks, ensuring that the patient can perform them safely and efficiently․ These may include squats, lunges, step-ups, and modified plyometric exercises, all performed with proper form and under the guidance of a physical therapist․
Activity-specific training tailors exercises to the patient’s individual goals and interests․ For example, a patient who enjoys gardening might practice lifting and carrying pots, while a golfer might work on their swing mechanics․ This approach not only improves physical function but also enhances motivation and adherence to the rehabilitation program․
Progression is gradual and based on the patient’s tolerance and progress․ The physical therapist carefully monitors the patient’s form, pain levels, and overall response to the exercises, adjusting the intensity and complexity as needed․ The ultimate goal is to restore the patient’s ability to participate fully in their desired activities, improving their quality of life and overall well-being․
Proprioception and Balance Exercises
Proprioception and balance are crucial for regaining stability and coordination after a Hip ORIF․ Proprioception, the body’s awareness of its position in space, is often compromised after surgery due to muscle weakness and altered joint mechanics․ Balance exercises challenge the patient’s ability to maintain stability in various positions, reducing the risk of falls and improving overall function․
These exercises begin with simple weight shifts and progress to more challenging activities such as single-leg stance, tandem stance (heel-to-toe), and balance board exercises․ The use of visual cues, such as focusing on a fixed point, can help improve balance initially․ As the patient progresses, exercises can be performed with eyes closed to further challenge proprioception․
The physical therapist carefully monitors the patient’s balance and stability during these exercises, providing support and guidance as needed․ Progression is gradual and based on the patient’s ability to maintain balance without assistance․ Incorporating proprioception and balance exercises into the rehabilitation program helps restore confidence, reduces the risk of re-injury, and improves the patient’s ability to perform daily activities safely and efficiently․ The ultimate goal is to regain dynamic stability and return to pre-injury levels of function․
Long-Term Considerations
Long-term considerations after hip ORIF include returning to activity, managing potential complications, and adhering to a home exercise program․ Consistent exercise and vigilance are crucial for sustained recovery and well-being․
Return to Activity and Sports
Returning to activity and sports following a hip ORIF requires a carefully planned and progressive approach․ The primary goal is to regain pre-injury function and participation levels while minimizing the risk of re-injury․ This process involves a gradual increase in activity intensity and duration, guided by physical therapist assessments and patient feedback․
Prior to resuming sports, individuals must demonstrate adequate strength, range of motion, balance, and proprioception․ Activity-specific training plays a crucial role, simulating the demands of the chosen sport or activity․ For example, athletes may engage in agility drills, plyometrics, and sport-specific exercises under the supervision of a physical therapist․
Close monitoring for pain, swelling, or other signs of overexertion is essential․ A phased return-to-sport program, customized to individual needs and abilities, ensures a safe and successful transition back to desired activities․ This approach focuses on restoring confidence and optimizing performance while protecting the healing hip joint․
Potential Complications and Management
While hip ORIF is generally successful, potential complications can arise․ These include infection, non-union or malunion of the fracture, avascular necrosis of the femoral head, and implant failure․ Early recognition and management are crucial for optimal outcomes․ Signs of infection, such as increased pain, redness, swelling, or drainage from the incision site, require prompt medical attention;
Non-union or malunion may necessitate further surgical intervention․ Avascular necrosis, a condition where the bone tissue dies due to lack of blood supply, can lead to hip pain and functional limitations․ Management may involve pain medication, activity modification, or, in severe cases, hip replacement․
Implant failure, although rare, can occur due to trauma or excessive stress on the hardware․ Physical therapy plays a vital role in managing these complications by focusing on pain control, restoring function, and preventing further deterioration․ Patient education on proper weight-bearing and activity modification is also essential․
Importance of Home Exercise Program
A consistent home exercise program is crucial for long-term success following hip ORIF․ It reinforces the progress made during formal physical therapy sessions and empowers patients to maintain their functional gains․ Adherence to the prescribed exercises helps improve strength, flexibility, and endurance, contributing to overall hip health and stability․ This program should be performed 2-3 times a day․
The home exercise program should be tailored to the individual’s specific needs and abilities, considering factors like age, activity level, and any underlying medical conditions․ It’s essential to follow the instructions provided by the physical therapist carefully, paying attention to proper form and technique to avoid injury․ Regular exercise helps manage pain, prevent stiffness, and improve circulation around the hip joint․
Patients should gradually increase the intensity and duration of their exercises as they progress, always listening to their body and avoiding any movements that cause excessive pain․ Consistent participation will ensure the ability to return to activities․